Cervical Disc Replacement
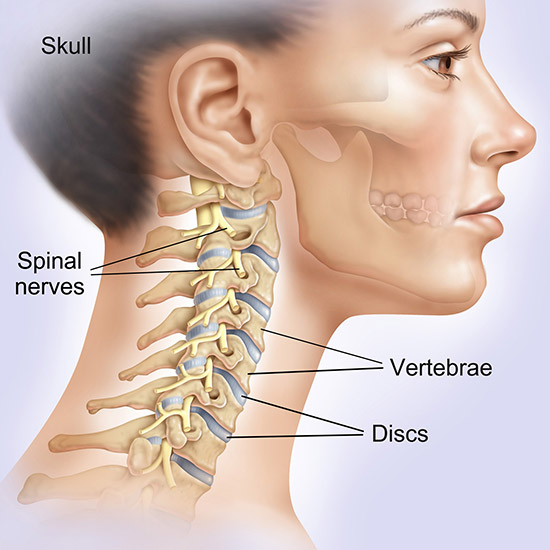
Artificial cervical disc replacement surgery is an alternative to spinal fusion surgery, where the damaged intervertebral disc in the neck is removed and replaced with a disc implant. This surgery relieves neck pain as well as restores the normal range of motion of the neck.
A cervical spine fusion surgery involves permanent fusion of two vertebral bodies and eliminates movement between them while an artificial disc is similar to the normal intervertebral disc and assists in movement.
Advantages
The advantages of the artificial cervical disc replacement include:
- Preservation of mobility
- Restoration of disc height
- Stabilization of the cervical spine
- Decreased stress during movement
- Supports the weight of the head, during rest and movement
Artificial discs are usually made up of a stainless steel and polyethylene combination. Some designs possess spike-like irregularities into the surface to enhance the hold over the upper and lower surfaces of the respective vertebral bodies. Bone screws are used to secure the artificial disc in place.
Indications and Contraindications
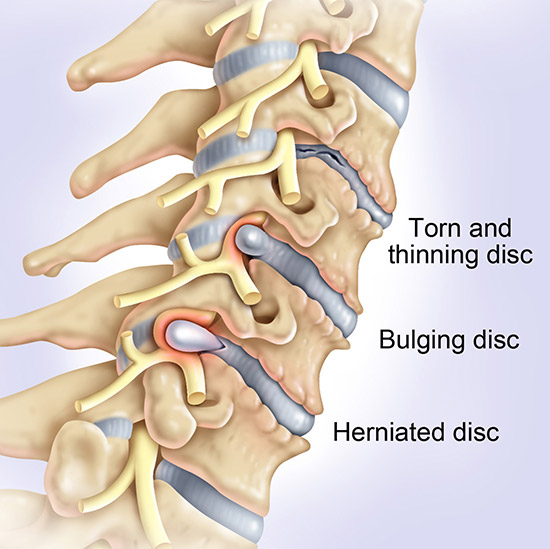
Artificial cervical disc replacement is usually indicated in the following circumstances:
- Progressive deterioration of your symptoms
- Neck pain associated with pain, weakness or numbness of the arm and leg
- Symptomatic cervical disc disease does not respond to conservative treatment
- Difficulty walking
Artificial cervical disc replacement is contraindicated in the presence of arthritis, significant osteoporosis or an active infection, and if the patient has allergy to stainless steel.
Procedure
Before the surgery your doctor will explain the benefits and risks of the device and the procedure to you. Your doctor may also order a few blood tests, X-rays, or other imaging tests to determine your medical condition. You may also need to obtain a health clearance from your physician for the surgery.
The patient is put under general anesthesia. The surgery is performed under X-ray guidance (fluoroscopy). You will lie face up on the operating table. Your surgeon approaches the cervical spine from the front of your neck. A small incision is made in the front of the neck and the soft tissues are gently retracted to access the cervical spine. The damaged disc along with any loose disc fragments or bone spurs are then identified and removed. After the disc is removed, the disc space is cleared and the artificial disc device is placed in the prepared disc space, restoring its normal height and relieving any pressure over the spinal nerves. The incisions are closed and covered with a dressing.
It is a minimally invasive procedure as the muscles and soft tissues are not excised during the surgery.
After the surgery
After your surgery, you will be transferred to a recovery room and the medical staff will closely monitor the vital signs. A cervical brace is recommended to offer stability and support during the healing process. You may experience mild discomfort, pain at the incision site, neck muscle spasms, or other related symptoms following the surgery.
Post-operative care
You will need to keep the incision area clean and dry. Refrain from hot tubs, swimming, heavy lifting, driving, and smoking. You can initiate physical therapy as directed by your surgeon. Take medications as recommended by your doctor. Arrange for a follow-up appointment with your doctor.

Risks
The potential risks associated with artificial disc replacement surgery may include infection, bleeding, nerve injury, and problems due to anesthesia.
Call your doctor if the incision site shows signs of infection such as pain, redness, swelling, or alteration in the quantity of smell of the drainage, or if you develop fever over 101° F. Also inform your doctor if you develop bowel and bladder dysfunction or numbness over the genital area.





